Prostate Cancer
Overview
Prostate Cancer begins when cells in the prostate gland ―gland found only in males that makes some of the fluid that is part of semen―, start to grow uncontrollably.
The prostate is below the bladder and in front of the rectum, and its size may change with age: in younger men, it is about the size of a walnut, but it can be much larger in older men.
Some prostate cancers can grow and spread quickly, but most grow slowly. In fact, autopsy studies show that many older men (and even some younger men) who died of other causes also had prostate cancer that never affected them during their lives. In many cases neither they nor their doctors even knew they had it.
Prostate Cancer is the most common cancer in men in the United States, after Skin Cancer. It is the second leading cause of death from cancer in men. Prostate Cancer occurs more often in African-American men than in white men. African-American men with Prostate Cancer are more likely to die from the disease than white men with Prostate Cancer.
Types of Prostate Cancer
There are several types of Prostate Cancers, but almost all are from the main type:
- Adenocarcinoma: a type of Prostate Cancer that develops from the gland cells (the cells that make the prostate fluid that is added to the semen)
Other types of cancer that also start in the prostate gland are:
- Sarcomas
- Small Cell Carcinomas
- Neuroendocrine Tumors (other than Small Cell Carcinomas)
- Transitional Cell Carcinomas
Risk Factors
Although we don’t yet completely understand the causes of prostate cancer, researchers have found several factors that might affect a man’s risk of getting it.
Risk factors widely accepted by the medical community for Prostate Cancer include:
- Age
- Race/ethnicity
- Geography
- Family history
- Gene changes
Other risk factors with less clear effect on Prostate Cancer include:
- Diet
- Obesity
- Smoking
- Workplace exposures
- Inflammation of the prostate
- Sexually transmitted infections
- Vasectomy
Symptoms and Signs
Early prostate cancer usually causes no symptoms. But more advanced prostate cancers can sometimes cause symptoms, such as:
- Problems passing urine, including a slow or weak urinary stream or the need to urinate more often, especially at night
- Blood in the urine
- Trouble getting an erection (erectile dysfunction)
- Pain in the hips, back (spine), chest (ribs), or other areas from cancer that has spread to bones
- Weakness or numbness in the legs or feet, or even loss of bladder or bowel control from cancer pressing on the spinal cord
Prognosis
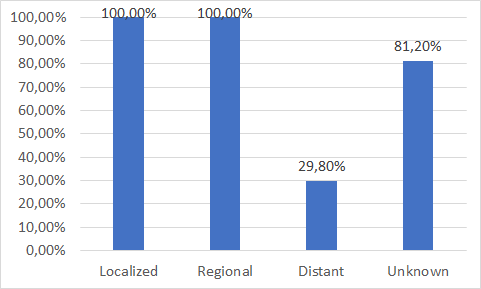
In stages I and II ―where there is no sign that the cancer has spread outside of the prostate― the relative 5-year survival rate is nearly 100%. About 4 out of 5 prostate cancers are found in this early stage. As long as the cancer has spread from the prostate to nearby areas ―cancers in sage III and IV― the relative 5-year survival rate for regional stage prostate cancer is nearly 100%. In more advanced IV stages that have spread to distant lymph nodes, bones, or other organs the chances to survive in the next 5 years is more or less 28%. As it can be interpreted by this data, the mortality associated to this kind of cancer is not very high since it has been detected before it is too late.
Prostate Cancer Diagnosis
PLEASE NOTE: EARLY DIAGNOSIS IN CANCER IS VERY IMPORTANT BECAUSE CANCER THAT’S DIAGNOSED AT AN EARLY STAGE, BEFORE IT’S HAD THE CHANCE TO GET TOO BIG OR SPREAD IS MORE LIKELY TO BE TREATED SUCCESSFULLY. IF THE CANCER HAS SPREAD, TREATMENT BECOMES MORE DIFFICULT, AND GENERALLY A PERSON’S CHANCES OF SURVIVING ARE MUCH LOWER.
As shown in the chart below, in Prostate Cancer, like many other cancers, mortality is substantially higher in patients whose disease is diagnosed in late stage or has metastasized to other organs.
State of the Art
Currently, Prostate Cancer diagnosis is done by a prostate biopsy (a test to remove small samples of prostate tissue to be examined under a microscope).
For a Prostate Biopsy, a thin needle is inserted through the rectum (transrectal biopsy), through the urethra, or through the area between the anus and scrotum (perineum). A transrectal biopsy is the most common method used. The tissue samples taken during the biopsy are examined for cancer cells.
A biopsy may be done when the PSA Test is performed and high levels of Prostate-Specific Antigen are found in blood, or after a Digital Rectal Exam (DRE) finds an abnormal prostate or a lump.
Unfortunately, PSA levels are also raised if Benign Prostatic Hypertrophy (BPH), Prostatic Infarction, Bacterial Prostatitis or Urinary Tract Infection.
Besides, some urological maneuvers have also effect on the level of PSA, such as:
- Rectal examination
- Prostate Massage
- Transurethral Resection (harvesting should be done after at least 6 weeks)
- Prostate Biopsy (harvesting should be done after at least 6 weeks)
- Ultrasound
- Cystoscopy
In a similar way, after hormonal therapy PSA does not always reflect tumor behavior, and Anti-androgen medication may cause low levels of PSA in the presence of residual disease.
Moreover, a prostate biopsy has a slight risk of causing problems, such as:
- Infection: This is more common in men who have undiagnosed prostatitis. Usually, taking antibiotic medicine before the biopsy prevents an infection from developing.
- Bleeding into the urethra or bladder: This can cause a blood blister (hematoma), an inability to urinate, or a need to urinate often.
- Bleeding from the rectum: If you have a transrectal biopsy, you may experience a small amount of bleeding from your rectum for 2 to 3 days after the biopsy.
- An allergic reaction to the anesthetic medicines used during the biopsy.
Diagnosis Revolution
Here is where our solution can help by being an innovative, non-invasive, accurate, and cost-effective diagnosis solution, based in a simple blood test that can detect Prostate Cancer with 81.7% of Sensibility and 98.2% of Specificity, while reduces ―in a very significantly way―, the number of false positives (FP) and false negatives (FN) typical of other diagnosis procedures.
If do you want to read more about OncoPROSTATE Dx, our Multiple Biomarkers Disease Activity Algorithms (MBDAAs) for an innovative, non-invasive, accurate, and cost-effective Prostate Cancer diagnostics, please click on next button: